MARYLAND MATTERS: After more than three years and 1.1 million deaths, the United States on Thursday ended the public health emergency for COVID-19 — and Congress is attempting to better prepare for a possible resurgence of that virus or another.
The expiration of the designation, originally put in place in January 2020, means alterations to how vaccines, tests and therapeutics are purchased and administered, though not all changes will take effect immediately. Less information will be available from the federal government about the frequency of the disease.
The emergency designation sunsetting marks something of an end to the pandemic, even though COVID-19 still remains active and will likely continue to evolve into new variants in the months and years ahead.
Rebecca Fischer, assistant professor of epidemiology and biostatistics in the Texas A&M University School of Public Health, said she expects infections, hospitalizations and deaths will mirror what the country has experienced under the public health emergency.
“What we’ve learned is, the unpredictable nature of COVID is something we can rely on,” Fischer said.
The change in status, she said, will allow officials to look back at what they’ve learned throughout the pandemic while preparing for a future where something similar could take place.
“The end of the public health emergency declaration makes it really important to take inventory of where we are with resources, infrastructure, staffing and training so that we can ramp up those areas,” she added. “So that when something unpredictable happens, such as a variant emerges or more severe illness happens, we will be better prepared to tackle those challenges.”
Cases and deaths from the virus continue to trend downward, though each week there are nearly 80,000 new diagnoses and more than 1,100 deaths, according to the Centers for Disease Control and Prevention
Vaccination rates have continued to wane the longer the pandemic has dragged on, with fewer than 17% of people getting the updated bivalent vaccination booster, compared to nearly 70% of Americans receiving their original two-dose vaccinations.
COVID-19 vaccinations, tests, treatments
Federal public health officials maintain that for many following the end of the public health emergency, vaccinations will continue to be available without charge through private insurance, Medicare and Medicaid.
The Department of Health and Human Services wrote in a fact sheet on the end of the public health emergency that “when that transition to the traditional health care market occurs, to protect families, the Administration has facilitated access to COVID-19 vaccines with no out-of-pocket costs for nearly all individuals and will continue to ensure that effective COVID-19 treatments, such as Paxlovid, are widely accessible.”
Uninsured people will continue to have access to the vaccine after the country transitions out of the emergency through a so-called bridge program, according to HHS.
Treatments for COVID-19, such as Paxlovid and Lagevrio, could cost more, depending on health insurance status. Medicaid patients will continue having access to treatments through Sept. 30, 2024, without having to pay.
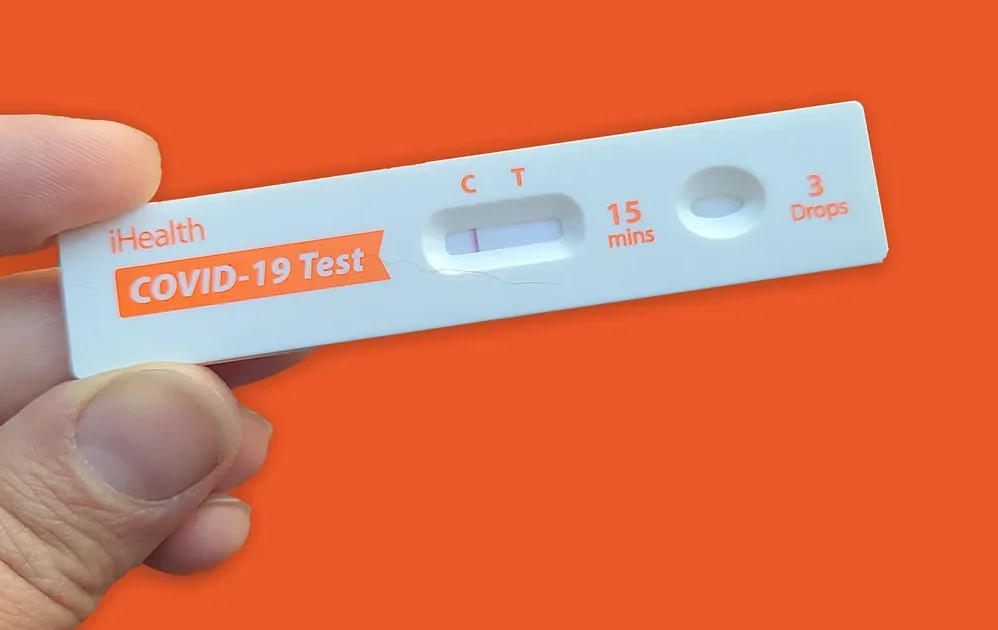
Access to free testing for COVID-19, either through a lab or at-home rapid tests, will change, though HHS says the federal government is keeping a stockpile and will mail free tests to people until the end of May through COVIDtests.gov.
“The requirement for private insurance companies to cover COVID-19 tests without cost sharing, both for OTC and laboratory tests, will end at the expiration of the PHE,” the fact sheet says. “However, coverage may continue if plans choose to do so. The Administration is encouraging private insurers to continue to provide such coverage going forward.”
Less COVID-19 data
The CDC will lose access to information about the percentage of COVID-19 infections with the end of the public health emergency.
The agency will no longer be able to require laboratories to report the number of negative tests, and the reports on hospitalizations from the virus will move from daily to weekly.
CDC Director Rochelle Walensky testified before Congress earlier this month that the end of the public health emergency “means that CDC will no longer be able to collect data and share information many Americans have come to expect.”
“We will make do, however this should worry us all — primarily because of what it says about the visibility we will have into the next outbreak,” Walensky said. “We will be back to square one, having to build and negotiate surveillance capacity while we fight a pathogen.”
At the beginning of the COVID-19 pandemic, she noted, it took the CDC about six months “to negotiate data use agreements in order to receive hospitalization data.”
During that hearing in the U.S. Senate Health, Education, Labor and Pensions Committee, Chair Bernie Sanders highlighted the likelihood of another public health emergency.
Sanders, a Vermont independent, will be at the forefront of that work as Congress looks to reauthorize the Pandemic and All-Hazards Preparedness Act this year.
“What scientists are telling us is that there is a reasonable chance that — God forbid — a pandemic as deadly as COVID-19 could occur in 10 years,” Sanders said. “All of us hope that that will not occur, but our job is to make sure that we are prepared if it does occur.”
Fischer, from Texas A&M University, said during a phone interview that spillover events, where an illness transfers from animals to humans, are “not becoming fewer and farther between but the opposite.”
“We now know a lot about respiratory spillover, which very well could happen again and how that might play out,” Fischer said, adding that public health officials could use that information to prepare for the next public health emergency.
“Next thing could be a hurricane,” she said, noting natural disasters also bring infectious diseases. “Our preparedness plans don’t need to be specific for a respiratory virus, though that could be one scenario.”
Getting better at preparation
Louisiana Sen. Bill Cassidy, the top Republican on the HELP Committee, said during the hearing that the Pandemic and All-Hazards Preparedness Act, or PAHPA, was “first enacted in 2006 largely to address the failures of the federal response following Katrina.” Hurricane Katrina in August 2005 devastated Gulf Coast states.
The law, Cassidy noted, established the Administration for Strategic Preparedness and Response, or ASPR, as well as the Biomedical Advanced Research and Development Authority, or BARDA.
Congress reauthorized the law in 2013 and 2019 and is tasked with doing so again this year, in the shadow of the COVID-19 pandemic.
“As we saw during the COVID-19 response, the PAHPA framework is far from perfect,” Cassidy said. “Poor management and maintenance of the Strategic National Stockpile meant that doctors and nurses were forced to use expired PPE.”
“One picture I remember is a huge quantity of masks being dumped right as the pandemic was starting because they were two weeks from being expired,” he added.
Utah Republican Sen. Mitt Romney and Pennsylvania Democratic Sen. Bob Casey will lead the effort along with members of the committee, Cassidy noted.
That reauthorization, he said, should improve on the last.
“We made mistakes, we learned some tough lessons, so let’s work together to make it so that next time it isn’t on the fly that we’re figuring it out,” Cassidy said. “Rather, there are systems that we can put into place, update the playbook and make sure that whatever we do, it’s flexible enough to address the threats beyond just a pandemic.”