Maria Vicente has no health insurance. During five pregnancies the only time she saw a doctor was in the delivery room. She lost two children from lack of prenatal care and complications giving birth.
The 37-year-old fled poverty in Guatemala for a better life in the United States. Since immigrating in 2006, she has worked as a housekeeper or in construction, as does her husband, when jobs are available and they are healthy.
Vicente volunteers to distribute food to people in need like herself, whose lives have been upended by pandemic-related social, economic and health issues, which hit her majority Latino community in Prince George’s County particularly hard. According to the Maryland Department of Health, Langley Park has consistently had the highest COVID incidence rates in the state.
Vicente has multiple health problems including diabetes. Between her frontline work and food deliveries, she contracted COVID four times. A ruptured appendix while pregnant nearly killed her. Multiple surgeries saved her life, but not her child’s. The operations left her in physical and emotional distress, and $38,000 in debt.
“The bills keep coming,” she said, upset she cannot pay them.
While Vicente’s children, born in the United States, have medical insurance, she and her husband do not.
“When you are undocumented, you are not eligible for health care,” she said. “I can’t apply for Medicaid, and I can’t apply for the Affordable Care Act, even though I might meet all of the other requirements.”
Maryland’s uninsured rate is at an historic low at 6%, down from 13-15% in 2000.
“The Affordable Care Act is a huge part of that,” said Suzanne Schlattman, deputy director of Maryland Health Care for All Coalition, the state’s largest health care consumer organization. She also credits legislative measures including subsidies for youth, easy enrollment to help with signups, a reinsurance program to keep costs from skyrocketing and new state funding for locally designed efforts to remove barriers to care in communities with documented health disparities.
However, none of the federal programs or these state’s initiatives for the uninsured population include undocumented Marylanders, which number 275,000 according the American Immigration Council.
Consequently, the care options open for undocumented immigrants are costly private insurance, hospital emergency rooms, online information or free clinics.
Vicente has tried them all. “It is hard or impossible to make an appointment [at the clinics], and they don’t offer everything,” she lamented.
Healthy Babies Equity Act expands some care
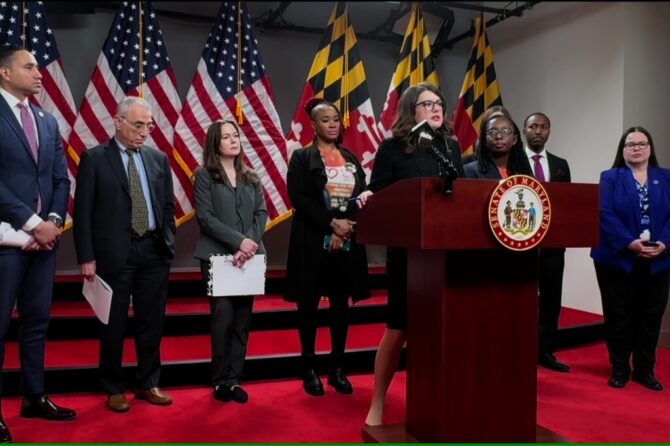
During the Maryland General Assembly session that ended last month, CASA mobilized behind two health care bills: the Access to Care Act, which wasn’t voted out of committee, and the Healthy Babies Equity Act, which passed with a veto-proof majority and will go into effect on July 1 without the signature of Gov. Lawrence J. Hogan Jr. (R).
“Immigration status should not be a barrier to receiving life-saving care, for mothers, for their children, for anyone, period,” said Cathryn Paul, government relations and public policy manager at CASA, the largest Latino and immigrant advocacy organization in the Mid-Atlantic.
The Healthy Babies Equity Act, which passed the General Assembly in March along mostly party lines with Republicans opposed, expands Medicaid to cover prenatal and postpartum care to pregnant people regardless of immigration status. Seventeen other states, including Virginia and Texas, provide coverage to pregnant people regardless of immigration status through Medicaid or other state-established programs.
Del. Joseline Peña-Melnyk (D-Prince George’s and Anne Arundel), the new chair of the House Health and Government Operations Committee, was its lead sponsor.
“This bill will reduce pregnancy complications and adverse fetal outcomes and the associated costs with it,” she said.
Under current law, the Maryland Department of Health provides Medicaid coverage for emergency medical services — including labor and delivery — for low-income undocumented residents who would be eligible for coverage but for their immigration status. The state also provides coverage for the first year of a child’s life if their mother was covered by Medicaid at the time of birth.
Last year, more than 5,000 undocumented immigrant women gave birth in the ER, at a cost of $89 million, about 50% covered by federal funds.
The bill passed this year would require the state to apply to the federal government for an expansion of Medicaid, which is expected to increase the federal reimbursement rate to 65%. Overall, legislative analysts estimated that the prenatal and postpartum care expansion would increase state spending by about $14.8 million, though a higher federal reimbursement for labor and delivery would mostly offset those costs.
The state could also see additional savings if the prenatal care reduces pregnancy complications and early childhood health issues, analysts said.
Vicente testified in favor of the bill, which was also backed by a coalition of faith, medical and civil rights groups. Advocates gathered outside the State House every day during the final days of the legislative session to press for the bill’s enactment.
Vicente told her story over and over.
“I did it for [immigrant] women, to make sure that what happened to me, won’t happen to them. I had no prenatal care. These women will. I am super happy about that,” she said.
“It was the strength and power of those individuals that legislators had to see and hear in person, that every person deserves life-saving and critical care regardless of their immigration status,” Paul said.
Counties taking action
Peña-Melnyk said policies to address inequity “should include all communities, and undocumented immigrants should not be excluded from [those] aimed at expanding access to health care.”
Local jurisdictions are following her lead.
Earlier this month, Howard County announced it would allocate $1.3 million in its next annual budget to support underinsured and uninsured mothers and pregnant people with access to health care, regardless of immigration status.
In ongoing budget negotiations in Prince George’s County, Councilwoman Deni Taveras (D) is working with the Alsobrooks administration to increase the county’s commitment to its Federally Qualified Health Centers, making services available to immigrants regardless of status. She said the $5 million from county coffers last year was gone in six months, based on a recent briefing provided by the county’s health department.
“For the program to be truly funded, it really needs to double the amount to $10 million,” Taveras said.
On broader statewide policies, Peña-Melnyk isn’t letting up.
“I want to promote health equity through policies that don’t traditionally focus on medical care, but have an equal, if not more important impact on health outcomes,” she said. “We need to provide equitable access to healthy foods, safe homes, to high-quality education and job opportunities. I want to use this framework in my mission to advance health equity for all communities in Maryland, especially those who have been marginalized and overlooked.”
CASA and its allies are considering their next steps to extend health care access for all. “This will be our priority until legislators meet the demands of this moment,” Paul said.
It is also Vicente’s passion.
“In this country, health care is a right that I will continue to fight for,” she said.
This article is from Maryland Matters, to read more stories like this click here.
Photo: Advocates gathered on Lawyers’ Mall every day in the last few weeks of the General Assembly session to advocate for passage of the Healthy Babies Equity Act, which was voted into law. Photo courtesy of CASA.